The Council of the College of Nurses of Ontario (CNO) relies on strong nurses and public leaders to provide policy leadership and oversight, to help ensure CNO is resolutely focused on its public protection mandate.
This June, CNO welcomes some new faces to Council, and some familiar faces to new roles — like Naomi Thick, who assumed the role of President this month. As President, Thick, along with peers on Council, will provide expertise to CNO’s work, helping to shape nursing regulation and promote safe nursing practices for generations to come.
A member of Council since 2017, Thick was previously Vice-President, RN, from 2020 to 2022. She’s a Clinical Manager in the Hematology & Oncology, MDU & Dialysis program at the Children's Hospital of Eastern Ontario (CHEO) in Ottawa. CNO sat down with Thick via Zoom to hear about her nursing journey so far, to talk about her goals for Council and to learn how a stop in Somalia gave her the confidence to take on any challenge.
CNO: Hi Naomi! Like all nurses, we know you are busy, so let’s start with, why did you become a nurse?
NT: I actually wanted to be a veterinarian until Grade 11! But only because my best friend wanted to be a vet. I eventually realized I had no idea what I wanted to do. I knew I wanted to be able to travel, be able to work anywhere and it had to involve people. I had a strong science background, and nurses are always needed. Before I got into it, I really had no concept of what nursing was, aside from what you see on TV. Which, if we’re being honest, is not real life! But then, I fell in love with nursing. I love every aspect of nursing that I have been part of.
CNO: Tell us a bit about your nursing career so far.
NT: I grew up on the East Coast and did my nursing education at Dalhousie University in Halifax. My first job post-graduation was on the oral maxillofacial surgery floor at the Queen Elizabeth II Health Sciences Centre.
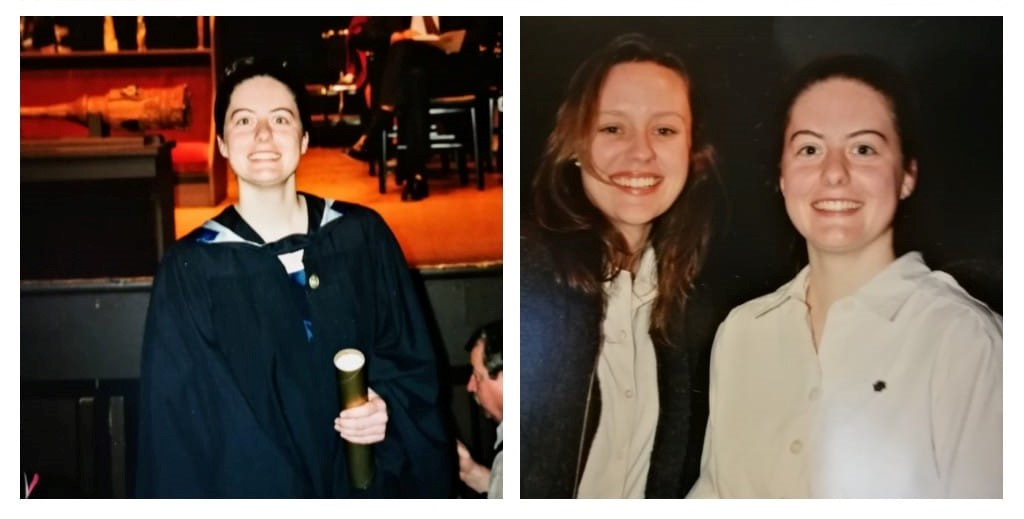
Thick at her graduation and pinning ceremony.
I really wanted to be able to work to full scope as a nurse, so I went up north to Wabasca- Desmarais, which is a small town about four hours north of Edmonton, Alberta. There’s a hospital and a small, predominantly Indigenous community there. It’s an industrial town — the population doubles or triples in the winter when folks come to work in the oil field, or in logging. We had 15 in-patient beds and the health care team was mostly nurses. There were physicians and we had X-rays and a lab, but there was no other auxiliary support. No physical, occupational or speech therapy — people were flown out if they required those services.
I worked really closely with an LPN — that’s the Alberta version of an Ontario RPN. On a typical night shift, it would be the two of us and no one else. During the day, there would be one other nurse. So, we did it all. The whole lifespan of a patient. You delivered babies and held people's hands at the end of life. There was lots of emergency care. It was trial by fire.
When I look back now, I see how lucky I was, because I was this new grad, and I had this LPN, who was so strong clinically, take me by the hand. We worked really well together. And there was always someone on-call I could phone with a question. As far as building my clinical skill set, it was tremendous.
After that, it had always been a dream to work with Doctors Without Borders. I did an eight-month stint in Somalia. I was the Nurse Manager of the medical team, and later the Medical Team Lead, accountable for all the 100+ beds that we had in the Health Centre. I got to work with people from all over the world.
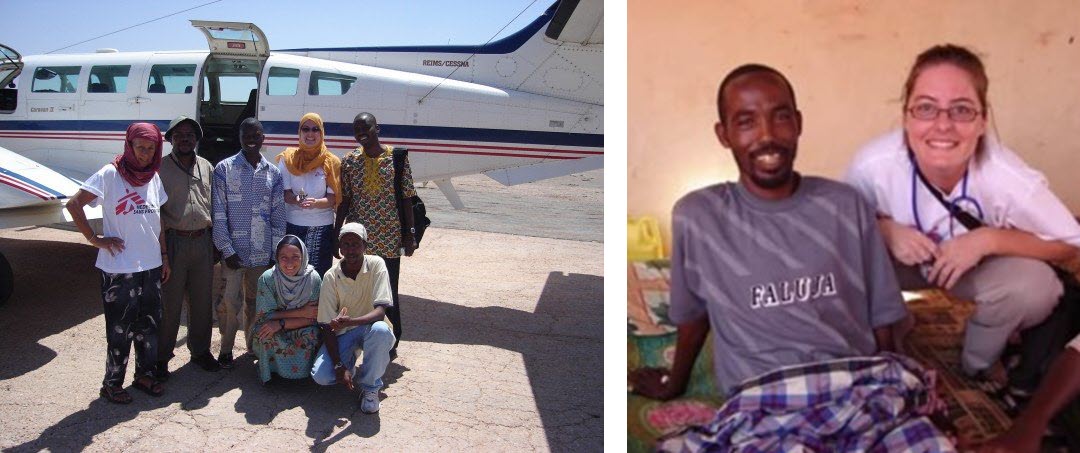
Thick with Doctors Without Borders in Somalia.
When I returned to Canada, I moved to a fly-in community out of Fort McMurray called Fort Chipewyan, in Alberta. It was a nursing station with a permanent population of about 700 people. I was the Chronic Care Nurse and got to do a lot of great community care, especially work involving lifestyle programs, including implementing a new Coronary Health Improvement Program.

Fort Chipewyan nursing station, 727 kilometers north of Edmonton, Alberta.
Then my husband got transferred to Ontario for his work, so I started working as an emergency nurse at Winchester Hospital.
CNO: You’re now a Manager at CHEO. When did you make the move into management?
NT: At Winchester. I’d just finished my master’s degree and felt like it was a role I could make a difference. I was warned in my interview about some of the historical challenges and the anticipated future challenges, but I figured I would give it a shot.
At Winchester, I was involved in clarifying RN and RPN roles, MAID implementation, did a lot of work with Alternate Level of Care (ALC) and practice model changes. I was the Manager for medicine, the enhanced care unit, complex care, discharge planning, and maternity and child.
CNO: Wow. Not a short list.
NT: No, but that's often the nature of rural care. There were two of us managers, and we split it. I took inpatient, and she had the outpatient unit. My time in the north really prepared me to be able to answer and respond to so many different areas.
I was there for six years, then I came to CHEO. I wanted to try my hat in a more urban centre. I've been at CHEO now for four years.
CNO: Why’d you get involved in Council?
NT: I am a firm believer that if you want to make system change, or if you have feedback about the system, then you need to get in the ring. I love the Theodore Roosevelt quote that Brené Brown uses: “It is not the critic who counts… the credit belongs to the man who is actually in the arena…” So, I put my name forward for Council.

Thick during a meeting of the Inquiries, Complaints, and Reports Committee.
CNO: And what was it like initially, when you joined Council?
NT: Not what I thought, actually! I don't think I really understood what regulation was. I knew CNO set the standards, and nurses who didn’t follow the standards could be disciplined by CNO. I did not grasp the scope of the work CNO does: approving education programs, quality improvement, all the processes around building the standards. I certainly didn't know all the work that was done at registration, or how closely you work within applicable legislation.
CNO: This is a familiar theme — we hear similar things from those joining our committees for the first time — it all connects back to the promotion of safe nursing practice and public protection!
NT: Yes. And it’s been amazing. I’ve loved being part of the process and seeing the whole system work. Since I’ve been on Council, the government has moved through scope of practice changes for every designation of nurse that CNO regulates. We went through the Long-Term Care Homes Public Inquiry, and then did a ton of work around abuse and serial killers in the health system.
CNO: Looking ahead now, what are you most looking forward to, as Council President?
NT: I'm really looking forward to how CNO is going to live out our commitment to diversity, equity, and inclusion (DEI). We've started the really early work, with doing our Land Acknowledgement and education for staff and Council, but there's a lot more that can be done. And, as the regulator who is tasked with patient safety and ensuring that nurses are providing safe care, we need to be a leader in articulating for nurses the role that DEI needs to play in patient care. Because DEI is not a “nice to have” — it’s an essential.
As well, I am really looking forward to realizing the full scope of our Governance Vision 2020. There are legislative changes that need to happen before we can fully implement it, but I’m so excited to execute this vision of using data to really see what is contributing to patient safety.
CNO:Final question. What would you tell a new grad or a nurse who's just entered practice? Any advice?
NT:People who are entering the profession right now are coming in during an ongoing pandemic. I know grads may feel unprepared because they didn't have as much clinical or practical experience, but here’s how you overcome that: focus on the patient in front of you.
You will learn just how adaptable to change you are; because practice does change, all the time, so that’s an important lesson to learn. Make sure you are listening to really strong experts and looking at what the data is telling you. Focus on the patient. Talk to your nursing colleagues — not just the ones working with you, but online too. Find your people. Find the ones who will call you up to greatness. This is a great career. Find your spot in it.
This interview has been edited for length and clarity.